Chapter 5: Child death reviews |
The Regulations relating to child death reviewsThe Local Safeguarding Children Board (LSCB) functions in relation to child deaths are set out in Regulation 6 of the Local Safeguarding Children Boards Regulations 2006, made under section 14(2) of the Children Act 2004. The LSCB is responsible for:
|
||||||||||||||||
|
|
|||||||||||||||
2. |
The responsibility for determining the cause of death rests with the coroner or the doctor who signs the medical certificate of the cause of death (and therefore is not the responsibility of the Child Death Overview Panel (CDOP)). |
|||||||||||||||
|
||||||||||||||||
3. |
The LSCB is responsible for ensuring that a review of each death of a child normally resident in the LSCB’s area is undertaken by a CDOP. The CDOP will have a fixed core membership drawn from organisations represented on the LSCB with flexibility to co-opt other relevant professionals to discuss certain types of death as and when appropriate. The CDOP should include a professional from public health as well as child health. It should be chaired by the LSCB Chair’s representative. That individual should not be involved directly in providing services to children and families in the area. One or more LSCBs can choose to share a CDOP. CDOPs responsible for reviewing deaths from larger populations are better able to identify significant recurrent contributory factors. |
|||||||||||||||
4. |
Other LSCBs or local organisations which have had involvement in the case should cooperate in jointly planning and undertaking the child death review. In the case of a looked after child, the LSCB for the area of the local authority looking after the child should take lead responsibility for conducting the child death review, involving other LSCBs with an interest or whose lead agencies have had involvement. |
|||||||||||||||
5. |
The LSCB Chair should decide who will be the designated person to whom the death notification and other data on each death should be sent.[56] LSCBs should use sources available, such as professional contacts or the media, to find out about cases when a child who is normally resident in their area dies abroad. The LSCB should inform the CDOP of such cases so that the deaths of these children can be reviewed. [56] List of people designated by the CDOP to receive notifications of child death information. |
|||||||||||||||
6. |
All forms and templates to be used for reporting child deaths can be found here: child death review forms. |
|||||||||||||||
7. |
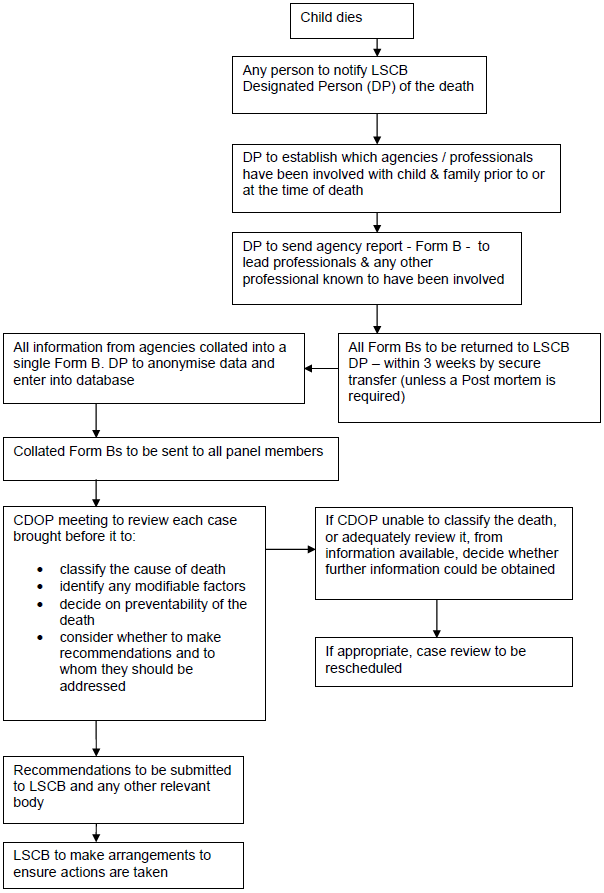
A summary of the child death processes to be followed when reviewing all child deaths is set out in flow chart 7 below. The processes for undertaking a rapid response when a child dies unexpectedly are set out in flow chart 8. |
|||||||||||||||
|
||||||||||||||||
8. |
The functions of the CDOP include:
|
|||||||||||||||
9. |
In reviewing the death of each child, the CDOP should consider modifiable factors, for example, in the family environment, parenting capacity or service provision, and consider what action could be taken locally and what action could be taken at a regional or national level. |
|||||||||||||||
10. |
The aggregated findings from all child deaths should inform local strategic planning, including the local Joint Strategic Needs Assessment, on how to best safeguard and promote the welfare of children in the area. Each CDOP should prepare an annual report of relevant information for the LSCB. This information should in turn inform the LSCB annual report. |
|||||||||||||||
|
||||||||||||||||
11. |
For the purpose of producing aggregate national data, this guidance defines preventable child deaths as those in which modifiable factors may have contributed to the death. These are factors defined as those, where, if actions could be taken through national or local interventions, the risk of future child deaths could be reduced. |
|||||||||||||||
|
||||||||||||||||
12. |
In this guidance an unexpected death is defined as the death of an infant or child which was not anticipated as a significant possibility for example, 24 hours before the death; or where there was an unexpected collapse or incident leading to or precipitating the events which lead to the death. |
|||||||||||||||
13. |
The designated paediatrician responsible for unexpected deaths in childhood should be consulted where professionals are uncertain about whether the death is unexpected. If in doubt, the processes for unexpected child deaths should be followed until the available evidence enables a different decision to be made. |
|||||||||||||||
14. |
As set out the Local Safeguarding Children Boards Regulations 2006, LSCBs are responsible for putting in place procedures for ensuring that there is a coordinated response by the authority, their Board partners and other relevant persons to an unexpected death. |
|||||||||||||||
15. |
When a child dies suddenly and unexpectedly, the consultant clinician (in a hospital setting) or the professional confirming the fact of death (if the child is not taken immediately to an Accident and Emergency Department) should inform the local designated paediatrician with responsibility for unexpected child deaths at the same time as informing the coroner and the police. The police will begin an investigation into the sudden or unexpected death on behalf of the coroner. The paediatrician should initiate an immediate information sharing and planning discussion between the lead agencies (i.e. health, police and local authority children's social care) to decide what should happen next and who will do it. The joint responsibilities of the professionals involved with the child include:
[57] PJ. Fleming, P.S. Blair, C. Bacon, and P.J. Berry (2000) Sudden Unexpected Death In Infancy. The CESDI SUDI Studies 1993-1996. The Stationery Office. London. ISBN 0 11 3222 9988; Royal College of Pathologists and the Royal College of Paediatrics and Child Health (2004) Sudden unexpected death in infancy. A multi-agency protocol for care and investigation. The Report of a working group convened by the Royal College of Pathologists and the Royal College of Paediatrics and Child Health. Royal College of Pathologists and the Royal College of Paediatrics and Child Health, London. www.rcpath.org |
|||||||||||||||
16. |
If the child dies suddenly or unexpectedly at home or in the community, the child should normally be taken to an Emergency Department rather than a mortuary. In some cases when a child dies at home or in the community, the police may decide that it is not appropriate to move the child’s body immediately, for example, because forensic examinations are needed. |
|||||||||||||||
17. |
As soon as possible after arrival at a hospital, the child should be examined by a consultant paediatrician and a detailed history should be taken from the parents or carers. The purpose of obtaining this information is to understand the cause of death and identify anything suspicious about it. In all cases when a child dies in hospital, or is taken to hospital after dying, the hospital should allocate a member of staff to remain with the parents and support them through the process. |
|||||||||||||||
18. |
If the child has died at home or in the community, the lead police investigator and a senior health care professional should decide whether there should be a visit to the place where the child died, how soon (ideally within 24 hours) and who should attend. This should almost always take place for cases of sudden infant death.[59] After this visit the lead police investigator, senior health care professional, GP, health visitor or school nurse and local authority children’s social care representative should consider whether there is any information to raise concerns that neglect or abuse contributed to the child’s death. [59] See footnote 48. |
|||||||||||||||
19. |
Where a child dies unexpectedly, all registered providers of healthcare services must notify the Care Quality Commission of the death of a service user – but NHS providers may discharge this duty by notifying NHS England.[60] Where a young person dies at work, the Health and Safety Executive should be informed. Youth Offending Teams’ reviews of safeguarding and public protection incidents (including the deaths of children under their supervision) should also feed into the CDOP child death processes. [60] Regulation 16 of the Care Quality Commission (Registration) Regulations 2009. |
|||||||||||||||
20. |
If there is a criminal investigation, the team of professionals must consult the lead police investigator and the Crown Prosecution Service to ensure that their enquiries do not prejudice any criminal proceedings. If the child dies in custody, there will be an investigation by the Prisons and Probation Ombudsman (or by the Independent Police Complaints Commission in the case of police custody). Organisations who worked with the child will be required to cooperate with that investigation. |
|||||||||||||||
21. |
In addition, for any child who dies in a secure children’s home, the Prisons and Probation Ombudsman will carry out an investigation. In order to assist the Ombudsman to carry out these investigations, secure children’s homes are required to notify the Ombudsman of the death and to comply with requirements at regulation 40(2) of the Children’s Homes (England) Regulations 2015 to facilitate that investigation.[61] [61] The Children’s Homes (England) Regulations are due to come into force on 1 April 2015. |
|||||||||||||||
|
|
|||||||||||||||
|
||||||||||||||||
22. |
If a doctor is not able to issue a medical certificate of the cause of death, the lead professional or investigator must report the child’s death to the coroner in accordance with a protocol agreed with the local coronial service. The coroner must investigate violent or unnatural death, or death of no known cause, and all deaths where a person is in custody or other state detention at the time of death. The coroner will then have jurisdiction over the child’s body until he or she releases the body for the funeral. Unless the death is natural, a public inquest will be held (and a public inquest will always be held where the death takes place in custody or other state detention).[62] |
|||||||||||||||
23. |
The coroner will order a post mortem examination to be carried out as soon as possible by the most appropriate pathologist available (this may be a paediatric pathologist, forensic pathologist or both) who will perform the examination according to the guidelines and protocols laid down by the Royal College of Pathologists. The designated paediatrician will collate and share information about the circumstances of the child's death with the pathologist in order to inform this process. |
|||||||||||||||
24. |
If the death is unnatural or the cause of death cannot be confirmed, the coroner will hold an inquest (and an inquest will always be held where the death takes place in custody or other state detention). Professionals and organisations who are involved in the child death review process must cooperate with the coroner and provide him/her with a joint report about the circumstances of the child’s death. Where possible, this should not be led by the clinician who was responsible for the care of the child when they died. This report should include a review of all medical, local authority social care and educational records on the child. The report should be delivered to the coroner within 28 days of the death unless crucial information is not yet available. |
|||||||||||||||
|
||||||||||||||||
25. |
Professionals should provide the coroner with all the evidence the coroner requires to carry out his or her statutory duty to establish who died, where, when and how. Coroners have a power (under section 32 and Schedule 5 of the Coroners and Justice Act 2009) to require someone to provide evidence to the coroner, or give evidence at an inquest. |
|||||||||||||||
|
||||||||||||||||
26. |
Although the results of the post-mortem examination belong to the coroner, it should be possible for the investigating paediatrician, pathologist, and the lead police investigator to discuss the findings as soon as possible, and the coroner should be informed immediately of the initial results. If these results suggest evidence of abuse or neglect as a possible cause of death, the paediatrician should inform the police and local authority children’s social care immediately. He or she should also inform the LSCB Chair so that they can consider whether the criteria are met for initiating an SCR. |
|||||||||||||||
27. |
Shortly after the initial post-mortem examination results become available, the designated paediatrician for unexpected child deaths should convene a multi-agency case discussion, including all those who knew the family and were involved in investigating the child’s death. The professionals should review any further available information, including any that may raise concerns about safeguarding issues. A further multi-agency case discussion should be convened by the designated paediatrician, or a paediatrician acting as their deputy, as soon as the final post-mortem examination result is available. This is in order to share information about the cause of death or factors that may have contributed to the death and to plan future care of the family. The designated paediatrician should arrange for a record of the discussion to be sent to the coroner, to inform the inquest of the cause of death, and to the relevant CDOP, to inform the child death review. At the case discussion, it should be agreed how detailed information about the cause of the child’s death will be shared, and by whom, with the parents, and who will offer the parents on-going support. |
|||||||||||||||
28. |
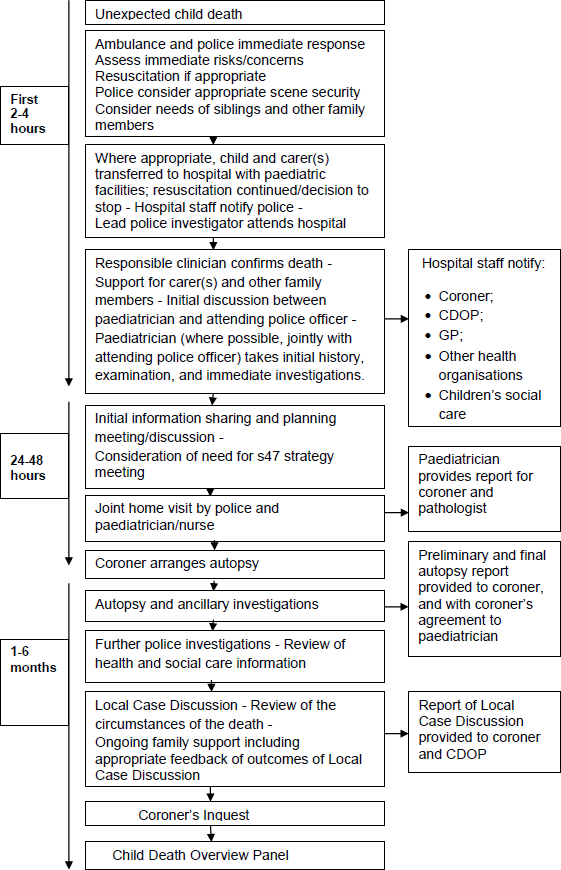
A flow chart outlining the process for response to the unexpected death of a child, flow chart 8.
|
|||||||||||||||
|
||||||||||||||||
|
||||||||||||||||
|
||||||||||||||||
|
||||||||||||||||